Thrombotic Microangiopathy
- +91 90537-79477
- nephrons2024@gmail.com
- Near Tinkoni, GT Road, Bathinda
Thrombotic Microangiopathy
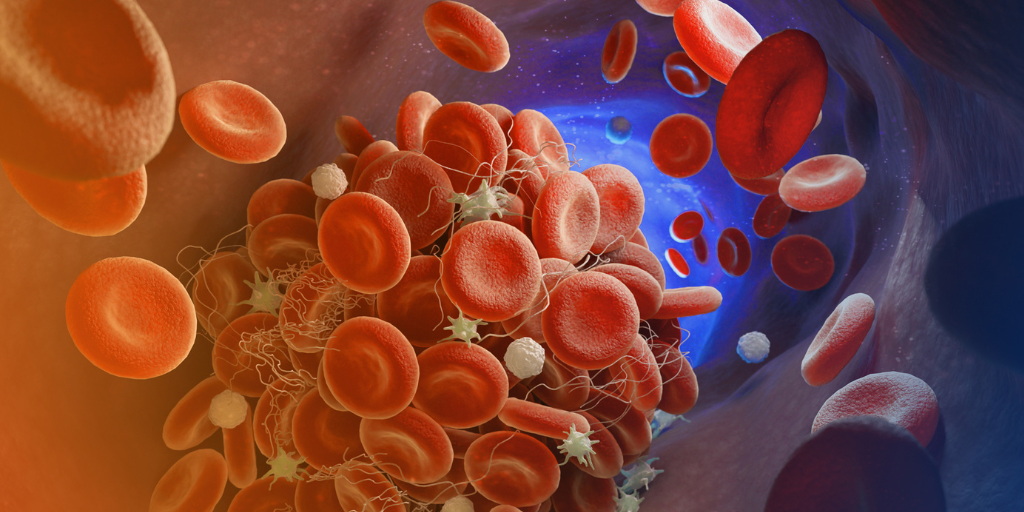
Thrombotic microangiopathy (TMA) is a broad term encompassing a group of disorders characterized by widespread formation of small blood clots (microthrombi) within the body’s smallest blood vessels (microvasculature). These microthrombi can damage various organs, particularly the kidneys, brain, and gastrointestinal system.
There are two main types of TMAs, each with a distinct underlying cause
- Hemolytic-uremic syndrome (HUS): Primarily affects children and is often triggered by an infection with Shiga toxin-producing E. coli (STEC) bacteria.
- Thrombotic thrombocytopenic purpura (TTP): Typically occurs in adults and is caused by a deficiency in a specific blood protein called ADAMTS13. In some cases, it can be triggered by certain medications or autoimmune disorders.
Let's delve deeper into each condition:
Hemolytic-uremic syndrome (HUS):
- Cause: Typically caused by STEC infection, which releases toxins that damage the lining of small blood vessels. This damage leads to microthrombi formation and subsequent:
- Hemolysis: Breakdown of red blood cells, leading to anemia and fatigue.
- Thrombocytopenia: Low platelet count, increasing the risk of bleeding.
- Acute kidney injury: Damage to the kidneys from microthrombi in the small vessels.
Thrombotic Thrombocytopenic Purpura (TTP):
- Cause: Deficiency in a blood protein called ADAMTS13. This protein normally breaks down large von Willebrand factor (vWF) multimers, which are sticky molecules involved in blood clotting. In TTP, a lack of ADAMTS13 allows large vWF multimers to persist, leading to:
- Microthrombi formation: Large vWF multimers can clump together and obstruct blood flow in small vessels, causing microthrombi formation.
- Thrombocytopenia: As platelets get used up in microthrombi formation, their count drops significantly.
- Organ damage: Microthrombi can damage various organs, particularly the brain (seizures, confusion), kidneys (acute kidney injury), and heart (chest pain, shortness of breath).
Similarities between HUS and TTP:
Both share the clinical triad of:
- Hemolytic anemia
- Thrombocytopenia
- Organ damage (often affecting the kidneys)
Differences between HUS and TTP:
- Cause: HUS is typically triggered by infection, while TTP is caused by ADAMTS13 deficiency.
- Age of onset: HUS primarily affects children, while TTP typically occurs in adults.
- Severity of kidney involvement: Kidney failure tends to be more severe in HUS compared to TTP.
Diagnosis of TMA:
Diagnosis of TMA involves a combination of:
- Clinical presentation: Symptoms like fatigue, easy bruising, bloody stools, and confusion.
- Blood tests: Checking for anemia, low platelet count, and abnormal markers of hemolysis.
- Urinalysis: Presence of blood or protein in the urine can indicate kidney damage.
- Blood tests for ADAMTS13 activity: Low levels suggest TTP.
- Imaging studies: May be used to assess organ damage.
Treatment of TMA:
Treatment depends on the specific type of TMA:
- HUS:
- Supportive care: Managing fluid balance and electrolyte levels.
- Dialysis: May be needed if kidney function is severely compromised.
- Antibiotics: Not effective against STEC toxin itself, but may be used to treat secondary infections.
- In severe cases, plasma exchange or medications to replace ADAMTS13 may be considered.
- TTP:
- Plasma exchange:** This is the mainstay of treatment, where the patient’s blood plasma is removed and replaced with donor plasma containing normal levels of ADAMTS13.
- Rituximab: A medication that suppresses the immune system and can help prevent further ADAMTS13 destruction.
- Plasmapheresis followed by ADAMTS13 replacement therapy: In some cases, this approach may be used.
Prognosis of TMA:
Early diagnosis and treatment are crucial for optimal outcomes. With prompt intervention, most patients with HUS recover completely. The prognosis for TTP is generally good with treatment, but some patients may experience relapses.
When to See a Nephrologist:
Consulting a nephrologist is essential if you experience any symptoms associated with Thrmobotic Angiopathy. Early detection and diagnosis are crucial for effective management.
Enhance your kidney health expert treatment by the best nephrologist in Bathinda. Book a session or contact Us on WhatsApp now!